Qualitywatch
A Nuffield Trust and Health Foundation programme
Latest from QualityWatch
QualityWatch is a Nuffield Trust and Health Foundation programme providing independent scrutiny into how the quality of health and social care is changing over time.
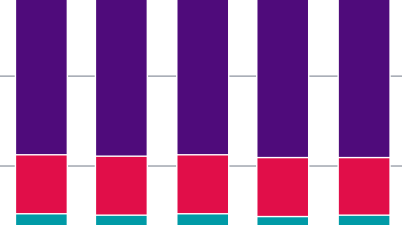
Declining access to social care
Read QualityWatch's annual statement, which focuses this year on access to adult social care. Presenting a range of key numbers and statistics to build a picture, it shows how the ability of the state to provide quality care that older people can access is changing for the worse.
Trending indicators
Here are some of our most popular indicators showing how care quality has changed over time. Head over to the 'Indicators' section to view them all alongside hundreds of other measures of quality in health and social care.
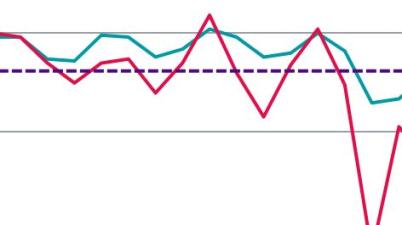
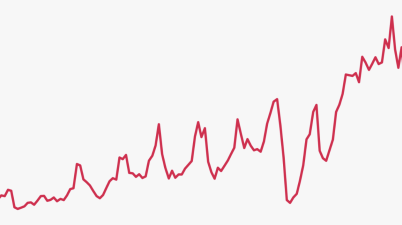
Cancer waiting times
Indicator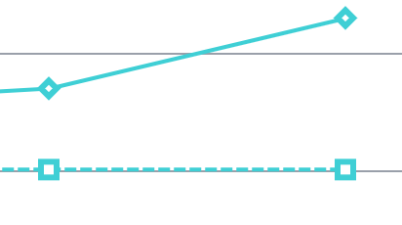
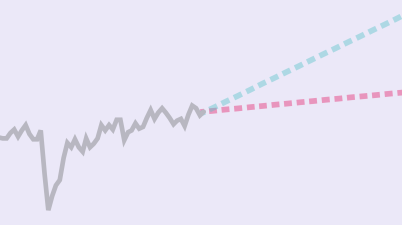
Ambulance response times
Indicator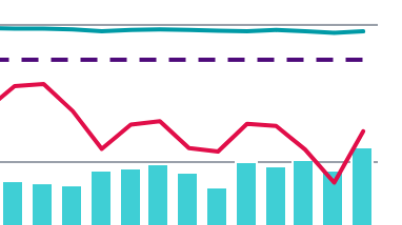
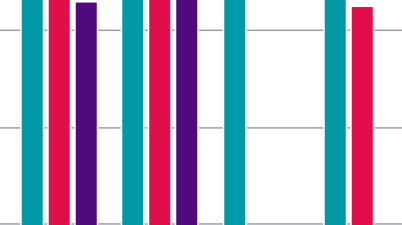
A&E waiting times
Indicator
Effectiveness of sexual health services
Indicator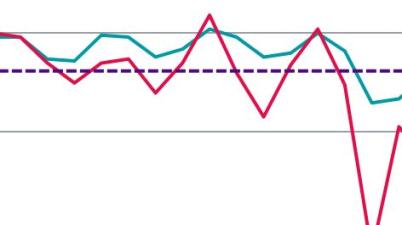
Cancer waiting times
Indicator
Effectiveness of sexual health services
Indicator